Introduction
Over the course of four separate cholera epidemics from 1883 to 1947, the British colonial government and its agencies closed access to water resources, forcibly entered homes and removed sick people from their families, ostensibly to prevent the spread of the disease. Government officials justified cholera sanitary measures as being in the best interests of public health. But the government relied on emergency methods that were reactionary, tactical, and did not benefit ordinary people. Rather, they furthered extractive colonial goals to control water, control bodies and police the private space of the home. In response, people resisted. This article highlights this archive of resistance through a series of sources, such as British government reports and Egyptian newspapers, that are widely available yet rarely studied.
Scientists had established a link between contaminated water and the spread of cholera as early as the global epidemics of the 1850s.1 British colonial sanitation practices in Egypt reframed lessons learned in the metropoles to complement the primary goal of controlling the powerful waters of the Nile and extracting its resources.2 During the cholera epidemics, this goal morphed into an effort to frame Egyptian sanitation practices, Egyptian water and Egyptian people as dirty, even dangerous. Official British reports brim with thick, affective descriptions about Egypt’s water. These claims were used to justify the aggressive and uneven implementation of invasive emergency sanitary measures. Authorities claimed that people resisted these measures because they did not know any better. However, this study, which focuses on the epidemics of 1883 and 1895–6, tells a more complicated story.
Locals resisted in numerous ways. They petitioned the state, they wrote letters to newspapers, they confronted officials in their offices and spread rumours. They hid their sick family members and their belongings, they fled their homes, they lied and persuaded others to lie.3 It is not difficult to understand why. The process of cholera home sanitation was to strip, chemically scrub and possibly burn belongings, and to remove gravely ill family members to hospitals or temporary cholera camps.
One example recorded in a report on the 1895–6 epidemic demonstrates the outcomes of home invasion under the auspices of disease control:
On visiting a house in which a death from Cholera had occurred, the body was almost invariably found lying in an empty room on the floor, every article of clothing, bedding, etc, had been removed. It was only after a systematic search that anything was found, sometimes in another room, sometimes in a neighbour’s house.4
In these episodes, the discovery of a cholera victim invigorates the pursuit rather than satiates it. The search, seizure and destruction of belongings, and the subsequent invasion of other homes follows. From this perspective, acts of resistance are reasonable.
Disease reveals uneven power dynamics and control measures were often strategic.5 In India and Egypt, for example, colonial politics inflected public health rhetoric, policies and enforcement.6 Cholera research likewise impacted the emerging field of public health. Laboratory science, such as chemical analysis and microbiology, was in development during this period and scientists used it to study cholera, as well as to suggest possible preventative measures and cures.7 Sanitary measures in any country unevenly impacted the poor and most vulnerable. Resistance was common, ranging from non-compliance to riots.8 The instances of resistance that I discuss are largely non-violent, the result of experience and rumour. As Luise White has shown, rumour was a culturally unifying force that had the power to communicate essential truths about the insidious cruelty of colonial governance as rooted in violence.9
My sources for this study are largely published or digitised archival material on the cholera epidemics, such as reports by the Public Works Department, the British colonial government, Egyptian newspapers and journals, literary sources, plans, maps and photographs. In British colonial reports, authors characterize resistance as ignorance.10 Egyptian elite representations of the same or similar resistance tactics varied. However, events of resistance read in pattern indicate that a significant architectural and spatial dynamic drove methods of control and resistance.
Cholera in Egypt
Cholera is a bacterial disease that can cause death in a matter of hours. Nineteenth-century accounts describe an extreme physical transformation as the body wilted, eyes and lips sank and the skin turned blue. Cholera victims suffered excruciating leg and stomach cramps and loss of speech. Uncontrollable vomiting and diarrhoea made the disease highly communicable.11 Caring for a sick person with cholera was a challenge in these circumstances and caring for the sick in Egypt during this time was done at home.12
In 1883, the epidemic struck hardest and killed upwards of 100,000 people.13 The British had invaded less than a year prior and many agencies and institutions were in disarray. By this time, medical research had linked cholera with contaminated water, but the miasma (bad air) theory prevailed in public health policy in the British colonies until the mid-1880s. Supporters of miasma theory were often politically motivated. If miasmas caused cholera, costly quarantines, water infrastructure modernisation and municipal reform could be avoided.14
British attempts to control the disease during the 1883 epidemic were haphazard. Messaging and methods were inconsistent and unevenly implemented. They targeted the poorest in cities and villages with sporadic enforcement of extreme measures, such as the destruction of a large area of Bulaq, a suburb of Cairo, by fire in August 1883.15 In other cities, such as Mansoura, the British colonial government imposed quarantines in the form of violent blockades that did not keep cholera from spreading, but caused many to die of other maladies, such as starvation.16 In Alexandria, officials interfered very little. Policies and practices favoured European populations in every locality, allowing them to bypass quarantine, and exempting them from sanitation measures. A French national suspected of cholera, for example, was allowed to recuperate at home under the care of a preferred doctor, and any attempt to address the individual about the disease had to be cleared through the appropriate consulate first.17 Native Egyptians, Ottomans and migrants from other North and Central African countries were not afforded such civility.
By the 1895 epidemic, the British had rearranged Egyptian health ministries and stripped them of local Egyptian and Ottoman Turkish control. They transferred most senior positions to British officers.18 Sanitary measures were strict, invasive and widespread, targeting water sources, streets, entire neighbourhoods and villages and private homes.19 The British knew that proper, comprehensive sanitation infrastructures, particularly proper sewer systems, were the best way to prevent cholera outbreaks. However, colonial policy favoured cheaper emergency measures. Indeed, a comprehensive sewer network was not installed in Cairo until 1907.20 British assumptions about the Nile, local water and water practice informed official claims about the epidemiology of cholera in Egypt.
Dirty water: critical visualisations of disease
The scientific process of isolating the cholera bacillus, linking it to water contamination and how this motivated specific sanitary reforms has been discussed elsewhere.21 In sum, it was a long and complicated process that was not linear, discrete or necessarily scientific. Politics and other interests informed research, treatment and other preventative measures. Cholera research was also global in scope, both in terms of geography and the nationality of medical professionals involved. In Egypt, a key thread that regularly appears in official government reports is the frequent characterisation of Egyptian water and water practice as unclean and even dirty.
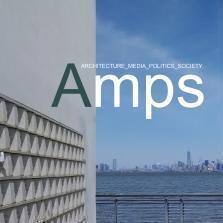
The 1883 and 1895–6 cholera epidemics began in Damietta, one of Egypt’s port cities located in the Nile Delta. At the time, Damietta was a small provincial capital of about 30,000 people. Its population had shrunk significantly after the cholera epidemics of the 1850s and endemic bovine typhus.22 Nevertheless, Damietta was an important provincial textile, basket-weaving and wood furniture-manufacturing centre that employed and served the local community.23 Like most Egyptian cities, the Nile served as its inhabitants’ main potable water source. Damietta’s elite favoured the views and climatic benefits of living close to the water (Figure 1). The city’s famous pilgrimage site, the Fatimid-era Mosque of Abul Ma‘ati, sat near a canal that encircled the city.
The city of Damietta on the Nile (Source: Douglas Sladen, ‘The City of Damietta on the Nile’ (1911), Rice University, https://hdl.handle.net/1911/21621)
After cholera broke out in Damietta at the end of June 1883, a series of commissions were dispatched to investigate. One of these was composed of British colonial medical doctors, including an official named J.W. Simpson who had previously served in a sanitation role in India. His report titled ‘Some Notes on the Cholera at Damietta’ is lurid and packed with boisterous rhetorical verve.24 Despite being certain that miasmas cause cholera, he is equally confident that the water practices of the local population are to blame. His negative affective tone leaves no doubt about his opinion. He describes Damietta’s water throughout his report as acrid, thick – even aspirating. ‘Green pools with gases bubbling up from them are seen in every part of the town. To me they were a source of anxiety, for I felt that I might be laid down with some malignant fever at any moment.’ Other descriptions seem to aim to prove that the people of Damietta revel in dirty water: ‘it was amusing to see the Arab children take off their scanty clothing, enter the puddles in the street, play, bathe, and roll in them, and come out covered from head to foot in a coating of mud and mire.’25
Simpson seems eager to establish a visible reason for cholera in Damietta in the form of dirty water. More than this, however, he claims that the residents of Damietta have little respect for water, contaminating the Nile and its canals with rotting bovine carcasses to save money and because it was easier than burying them:
[Officials] took out 400 putrid carcasses in one week … most … in such a decomposed condition as to make it impossible to drag them out of the river except in pieces. The work was of an intensely offensive and sickening nature … as they gradually accumulated they created a pestilential state … in the water.
This excerpt from Simpson’s account implies that Damiettans do not know mud from clean water, they contaminate their source on purpose and thus there is little hope for them. In his view, the town of Damietta and its residents are the inverse of modern sanitation. His graphic descriptions are vivid and aim to present the situation as doomed, even inevitable. Even more so, Simpson and his colleagues’ method, as described in official reports, of following water into homes and from home to home provides the basis for the more aggressive measures standardised by the 1895–6 epidemic. For Simpson: ‘whatever may have been the origin of cholera at Damietta, there is little doubt its rapid spread was mainly due to the defilement of the water.’26
Tepid accord: Egyptian elites parse cholera
Even as the British presented Egyptians and their water practices as ignorant, they were simultaneously relying on local resources, knowledge, expertise and labour. Educated Egyptian and Ottoman locals formed an important part of the infrastructure of cholera management, as doctors, lab analysts, police officers and support staff.27 There were also concerned residents who were well-informed about the latest in medical advances and sanitation practices.
Local intellectuals believed in ‘modern’ (understood as Western) sanitation and participated in the development and dissemination of its methods. However, proper sanitation had always been an important part of Egyptian and Ottoman culture.28 The framing of sanitation as a modern (Western) idea was partly a matter of scale but was mostly a social construct created to differentiate Egyptians (and other peoples outside Europe) from the coloniser.29 Thus, local elites played an important and complicated role in the dissemination, enforcement and public criticism of British colonial practices. As a group, they supported the science and the goals, but not necessarily the methods or manner of implementation.30
Another commission was sent to Damietta in 1883 by Hassan Mahmoud, the president of the Maritime Health and Quarantine Board. The leaders of this commission, medical doctors Ahmet Chaffey and Salvatore Ferrari, describe the results of their investigation in a 25-page pamphlet.31 They argue that the evidence concerning the cause of cholera is inconclusive and may have been due to the confluence of hot, humid weather and a festival – the mawlid (saint’s birthday) of Abul Ma‘ati – that drew about 15,000 people to the city. Their method is comprehensive, including fieldwork, chemical analysis of the water, a survey of the town, interviews with doctors and caregivers and an examination of local cholera victims. They come to similar conclusions as Simpson in the sense that they believe the town’s sanitation situation is a problem and aided the quick spread of cholera. They note standing water in houses, narrow damp lanes, many ruined structures used as dumping grounds and not enough lavatories and other infrastructure to support the crowds at the mawlid.32
Chaffey and Ferrari are clear, however, to mention the issue of unequal access to clean water when the Nile was low:
The only drink consumed by the inhabitants [of Damietta] is water. The rich save their water for seven months in a cistern, replenished by water from the Nile during the flood. But the inhabitants who do not have a cistern drink water from the river or the canal all year long.33
This is different from Simpson’s description, for example, which posits that all inhabitants have the same habits, regardless of resources.
Chaffey and Ferrari do not moralise about the situation or attempt to blame anyone in particular. The problem is systemic and comprehensive sanitary reform is necessary. They are quite clear that these considerations should be prioritised and not entangled with other reforms that the government is pursuing:
We conclude with a sincere wish that the immediate future will profit from the experience of the past to avoid fresh suffering. And that Egypt, prior to reforming its social and political institutions, will commence with that which is the basis of everything: Hygiene. 34
Chaffey and Ferrari clearly disagree with Simpson that the situation at Damietta is hopeless or the result of ignorance. They exhibit a more complex understanding of urban water infrastructure, resource management and the role of government in aiding those most vulnerable.
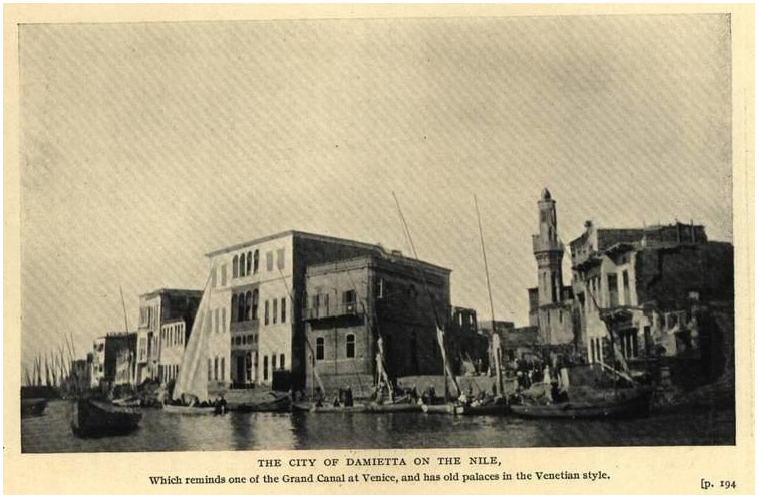
There was a robust public discourse in the Arabic-language popular press and periodicals on cholera, water, hygiene, public and private health. These appeared both during and outside times of crisis.35 Al-Muqtataf, especially, was a pre-eminent venue for the discussion and dissemination of scientific research, as well as more practical tips and advice (Figure 2).36
Detail, illustration of cholera bacilli in the intestine (Source: ‘Kalam al-Duktur Kukh fi al-Hawa’ al-Asfar’, al-Muqtataf 9, no. 2 (1884): 67 © British Library Board)
Egyptian and foreign elites shared the belief that sanitation in the home was a critical method to fight cholera.37 A growing literature over the course of the late nineteenth and early twentieth centuries provided advice on the prevention of any number of maladies, including cholera, through diligent personal hygiene practices. Authors advised concerned individuals to pay special attention to the entire home, notably by regularly cleaning dishes and water containers, furniture, bedding and clothing. Ventilation was also important, as was the proper type of air (dry, cool) for the sick. Al-Muqtataf’s editors prided themselves on publishing local and global research and perspectives, including contributions from Egyptians.38 In the pages of magazines, advice melded traditional water purification practices with the latest research and advances in personal hygiene technology.39
Controlling water
For sanitation officials, controlling water was necessary for several interconnected reasons. First, colonial officials and some members of the Egyptian elite believed that poor people, including local Egyptians and migrants, were responsible for the spread of cholera by contaminating the water. This is aptly expressed by Simpson’s report described above. This racist and largely unproven assumption actually caused sanitation conditions to worsen, as more people shared the same meagre potable and alimentation resources.40 Second, by denying public access to open water sources, the colonial government gained further direct control over the dissemination of a precious natural resource. This included the commodification of water, which was fundamentally anathema to Ottoman Egyptian water practices, which were not policed so that water was essentially free.41 Controlling water as a part of emergency sanitation practices was, in essence, part of a larger effort to turn water into a commodity. Part of this effort required the rhetorical classification of free water as dirty water.42
Officials used several methods to discourage and prohibit people from pulling water from the Nile and its canals during the cholera epidemics, such as distributing pamphlets condemning the practice as dangerous and providing limited access to filtered water from some corporate water taps for free.43 The Alexandria municipality required water carriers to always wear an official registration number. These badges were distinct colours for water carriers who pulled water from the Alexandria Water Company taps and those who pulled it from other sources, such as the Mahmudiya Canal. Failure to comply with any regulation ran the risk of penalties, including fines and potentially imprisonment if the fine could not be paid.44 Water carriers at both Cairo and Alexandria were also required to have their goatskin water sacks regularly disinfected by the sanitation authority.45
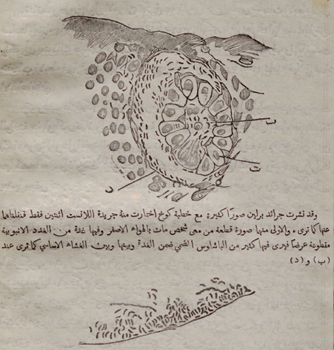
In Cairo, sanitation officials erected barriers at popular access points to the Nile and the Khalig al-Masri to deter professional water carriers and members of the public. Sources suggest that the primary reason for surveillance was to prevent people from washing their clothes or dumping waste or other matter into the water. Police officers or watchmen stood guard over closed and barricaded staircases, banks and informal landings.46 Officials targeted ponds, lakes and especially the Khalig al-Masri, the city’s main canal, as potential sources of disease (Figure 3).
In July 1895, a cholera outbreak in homes along the Khalig encouraged colonial officials to order it temporarily closed. They drained the water and disinfected it with lime: ‘The disinfection produced one excellent result, in that the people believing that the water was being poisoned by the Sanitary Department, refrained from using it. The end was thus attained.’47 Although the official who wrote these words sees people’s aversion to the Khalig as a positive outcome, the belief that the British were poisoning water was a powerful rumour that spread well beyond the confines of the canals.

Khalig al-Masri, Cairo’s main canal, photograph, circa 1895 (Source: Bibliothèque nationale de France, département des estampes et de la photographie, EI-182, https://gallica.bnf.fr/ark:/12148/btv1b53120159k)
Following water into the home: invasive sanitary measures to control ‘cholera’
Once sanitation officials discovered a person afflicted with cholera, they inspected and sanitised their dwelling. If the house was made of temporary materials or deemed too unsanitary, it might be destroyed. This was often the fate of dwellings called shacks (Arabic: ‘ishsha, pl. ‘ishish) (Figure 4).
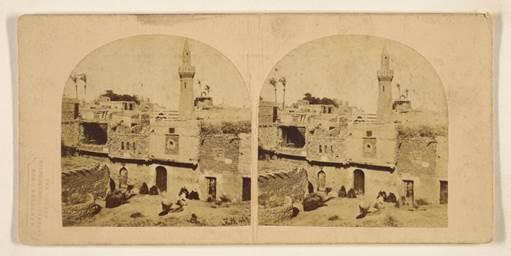
View at Boulac. The Port of Cairo, stereocard, 1856–7, Francis Frith (Source: The J. Paul Getty Museum, https://www.getty.edu/art/collection/object/107057)
Otherwise, a sanitation crew entered and followed a set of specific procedures. Day labourers paid a meagre wage were ordered to clean and disinfect containers; anything made from unsealed clay was likely to be destroyed. They disinfected furniture, bedding and all kitchen items with sublimate or lime solutions.48 Furnishings in sick rooms, such as the mattress or mat and any bedding or linens, were also likely to be burned. The walls up to 2 metres tall were washed and disinfected.
Residents would be forced to leave as the house was sanitised, and the cholera patient was usually sent to a hospital. Rumours about cholera hospitals were especially bleak and virulent. People claimed that cholera patients would first be incapacitated with chloroform on a yellow handkerchief, then at the hospital they would be left to die with no care, family members were not allowed to see them, nor were they even informed where the patient was taken. If the patient died (and rumours posited that this was the inevitable outcome), the body would be dissected, studied and buried without the proper rituals. Family members would not be informed and there would be no funeral.49
Outbreaks of cholera in Cairo and Alexandria required the construction of temporary cholera hospitals or camps to manage the sick (Figure 5).
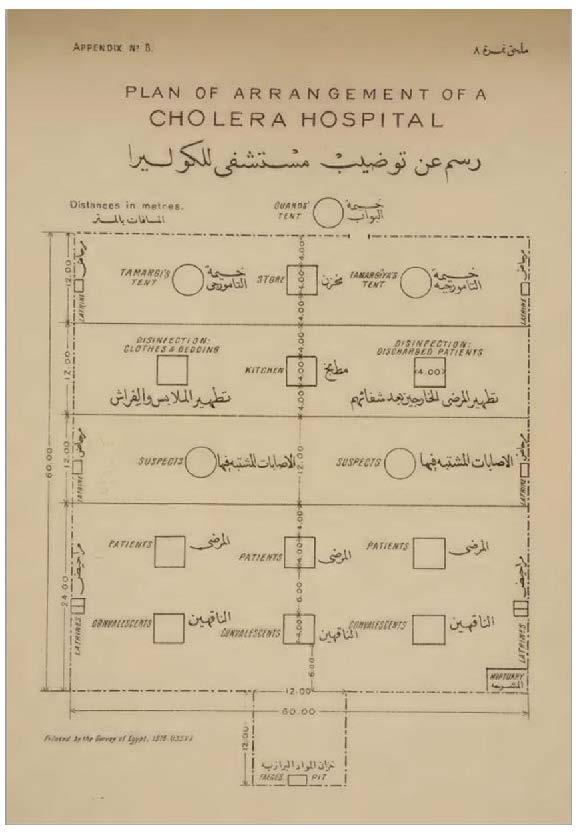
Plan of Arrangement of a Cholera Hospital (Source: Department of Public Health, Instructions on Procedure in Outbreaks of Cholera [Cairo: Government Press, 1918]; Wellcome Collection, https://wellcomecollection.org/works/rfy5tb7a)
Instructions for a plan for a temporary camp separates convalescents, patients and suspected cases, disinfecting stations and hospital attendants into a linear arrangement. There are separate tents for the male (tamargi) and female (tamargiya) hospital attendants. Each section has three to nine small temporary structures or tents. These are placed in the middle of each section, anywhere from 6 to 20 metres apart. The camp is fenced off and guards are stationed in a tent at the entrance, at the top of the plan in Figure 5. Confirmed cholera patients and convalescents are placed farthest from the guards, near the mortuary and faeces pit on the bottom of the plan. In the middle are suspected cholera patients, disinfecting stations and a kitchen. The hospital attendants’ quarters and a store are located closest to the entrance.
The linear plan aims to impose order on managing highly contagious disease and to control patients with the least amount of direct surveillance. One entrance constricts movement in and out of the camp. Those who present the greatest risk are placed at the back, farthest from the only entrance to the camp. Should they die, they are also close to the mortuary. The plan suggests that the removal of bodies and waste was a public affair, as there is no rear entrance to move them out of the camp surreptitiously. The sick and the healthy pass through the same spaces and along the same path. The mechanisms and arrangement of the plan turns ostensibly therapeutic spaces into landscapes of control, similar in design and modality to prisons, slave quarters and insane asylums.50
Photographs and descriptions of such hospital camps are rare. One example from 1895–6 shows such a station at Old Cairo, a suburb hit particularly hard during each epidemic (Figure 6).

Temporary cholera huts at Old Cairo (Source: Egypt, Ministry of the Interior, Sanitary Department, Report on the Epidemic of Cholera in Egypt during the Years 1895 & 1896 (Cairo: National Printing Office, 1897), 60. Courtesy: University of Chicago Library)
The camp is surrounded by high stone or brick walls, suggesting it was placed in the centre of ruins. The camp is composed of large windowless wooden structures with pitched roofs. A figure in white, perhaps a medical attendant, stands at the large entrance to one of them. In Tripoli during the 1911 epidemic, the Italian colonial government converted hotels and other structures to hold cholera patients. There are a handful of photographs of these camps at the Bibliothèque nationale de France and they depict shocking, inhumane conditions.51 In Andrée Chadid’s novel, Le Sixième jour, an account of the cholera hospital camps during the 1947 epidemic is one of the primary reasons that the main character, Sadikka, hides her grandson from the sanitation authorities when he is stricken with the disease. According to Saddika’s nephew, Saleh:
The hospital is the worst! … I made my way into one of the tents, it was horrible! The same face everywhere: blue, hollow, tongue hanging out. The patients lie next to each other in the sand, vomiting, two already dead and left there … A nurse came in wearing boots and a mask, he pushed me out before I could find my people … Never will I forget, since then we’ve hidden our sick and our dead!52
Articles in the local press debated the wisdom of resistance. A trident article from June 1896 thoroughly supported sanitation efforts and saw resistance as largely limited to the poorer classes.53 The author considers compliance or resistance in essentialist terms, as a binary between those who understand proper sanitation and respect the law, and those who are ignorant and are criminal. The author also notes that rumours about ill treatment and poisoning are perpetrated by peasants and children and ‘spread like lightning’.54 Still, others were vocally sympathetic towards resistance efforts. In one editorial titled ‘The Epidemic and Doctors’, the author argues that provincial doctors, especially, do not respect their patients, causing distrust and resentment: ‘If a patient arrives at the clinic, the doctor ridicules him for how he lives, scorns his dress, and insults his people.’55
Despite this debate, accounts of resistance ultimately show that sanitation measures were enforced across classes and that many, poor or otherwise, resisted:
[One] curious incident occurred when inquiry was made of a respectable man about his wife, who had died of cholera. First he said his wife died at a friend’s house; a few moments after he declared she had died at home, and possibly thinking he had been too definite, he finally remarked he really could not remember.56
The British official who noted the man as ‘respectable’ seems to have done so to suggest that all Egyptians are unreasonable and suspicious. But the reality of the situation was likely much more complicated. This respectable man and his household may very well have been following every common-sense sanitation measure. This would have decreased the likelihood of contracting the disease, but not erased the risk entirely. Either way, the man takes quick action to avoid enduring sanitation measures, or having his home invaded and his wife’s body taken. However, he seems to have realised that by placing his wife in any definite location he was inviting the colonial sanitation authority to enter there. Thus, he finally denies remembering the location of her death altogether.
In another account, an official discusses patterns of concealment:
The utmost ingenuity was displayed in the concealment of cases. On one occasion, the corpse of a cholera case was found in the oven covered with a heap of flour, which would have been used probably for the next day’s baking. On another, a case still alive was found doubled up in a small wardrobe. Cases were removed to the cotton and dhurra fields during the day, and brought back, alive or dead, to the house at night.57
In these examples, ordinary objects and spaces in the home become hiding places. Furniture and appliances aid attempts to subvert sanitation officials. No potential hiding place is overlooked; family and sanitation officials alike are aware of this. Indeed, during the 1947 epidemic, deceased cholera patients were found concealed in a cabbage cart.58 This extract also tells us about the ubiquity of resistance across households from different socio-economic classes. Those who cannot hide a sick family member at home take them elsewhere to keep them safe, to the cotton fields while they work and then return with them at night.
In another incident, an employee of the British Consul is questioned because he is visibly distressed. He abruptly admits that he is upset because his child died the previous evening of cholera, and his other children are also very ill. The man relates that he had not sought out a doctor as the children’s fate is in God’s hands. The consul insists that a doctor be sent for. The doctor arrives and after hearing the story suggests that an autopsy may be necessary to determine the child’s cause of death. The man becomes quiet. He then goes home and hides his other children, and afterwards denies saying anything about cholera or sick children. He also persuades members of the community to say the same, and to claim that the dead child had exhibited no symptoms of cholera at all.59
This shows that rejection of sanitation methods was widespread, extending to those who worked with the British. Rumours and the entreaties of neighbours superseded government codes and measures on pamphlets and in newspapers. He was also clearly more afraid of the sanitation authority entering his home than he was of possibly losing his job or any other related consequences of his actions, and used any tactic he could muster to keep the sanitation officials at bay.
Concluding remarks
Author and intellectual Taha Hussein was born into a modest but respected family in Upper Egypt. In his fictionalised autobiographical work, The Days, he describes his family experiencing cholera in 1902.60 Hussein writes that cholera ‘descended upon Egypt and attacked the population like wildfire. It destroyed towns, villages, and whole families.’61 The sanitation authority appears everywhere, closing schools and setting up tents and inspecting towns to isolate the sick.
‘Souls were filled with anxiety and hearts with fear. Life became a thing of no account for people. Every family talked about what had befallen the other and waited for their own share of disaster.’62 Hussein’s family is no different, and eventually his brother falls ill and dies.63 Hussein’s account emphasises what was at stake during the cholera epidemics: family, the lives of loved ones, the community. This fact is altogether muddled in other sources, even all of these make repeated appearances.
Rumours fuelled what experience affirmed: resolute resistance to any cholera sanitary procedure was necessary to preserve the community, its resources, its people. British sanitation officials and some Egyptian elites could only fathom that the reason for resistance was ignorance. Resistance efforts claim an alternative narrative: the community and family were the ones caring for the public, its health. The government and sanitation authority were engaged in ripping it apart. Knowledge passed through urban communal space primarily through experience, through informal communal networks that spread rumour for good reason. Reaction to cholera sanitary measures relied little on an individual’s intellectual understanding of the disease’s pathology. Rather, in the streets, courtyards, hallways, kitchens and fields of Egypt, the experience of the pursuit of cholera dictated methods of resistance.
There are two primary interdisciplinary lessons that we can take from this study. First, the control of resources, in this case access to water, is never neutral, nor is it naive. Government officials at the time understood that the control of water in the hinterlands and in the cities furthered the larger aims of colonial governance in Egypt, such as the commodification of potable water and the exploitation of water resources to increase cash crop yield. Not to mention that emergency measures rather than comprehensive sanitation reform were significantly cheaper and largely did not affect the European populations living in Egypt.64
Second, the history of resistance to disease control measures is historically implicated. The people of Egypt understood that the ones enforcing drastic sanitation measures, including home invasion and family separation, were the same people who had violently invaded and occupied the country. Similarly, during the Covid-19 pandemic, members of historically oppressed groups, such as Black Americans and Indigenous Americans in the United States were wary of vaccines and even loath to wear masks.65 In the latter case, community members expressed concern that masks would encourage invasive policing, much like hoods and other concealing clothing.66 If this is the case, what can be done in the future? Clearly the answer is not simple, nor can it be limited to transparent communication regarding disease prevention measures, vaccination research methods or the extremely difficult and uncertain process of epidemiological research. Indeed, repairing trust will be much more difficult and may require reparations the state is unwilling to concede.